Hair Transplant Results Timeline Month by Month: The Shock Loss to Final Density Journey
The decision to undergo a hair transplant represents a significant investment—not just financially, but emotionally. Understanding the complete journey from surgery day to final results helps patients navigate each phase with realistic expectations and reduced anxiety. This comprehensive guide examines the biological processes behind each recovery milestone, providing the knowledge needed to recognize normal healing patterns versus concerning signs.
Hair transplant results follow a predictable 12-18 month timeline, with graft survival rates of 90-95% when performed by qualified professionals. However, the path to final density involves distinct phases that challenge patience and test resolve. Crown results notably lag frontal results by 4-6 months—a critical reality often glossed over in standard timelines. This guide goes beyond surface-level information to explain the biological reasons behind each phase and provide practical documentation strategies.
Understanding the Three Emotional Phases of Hair Transplant Recovery
Rather than viewing recovery as simply a physical process, understanding the psychological journey helps patients prepare for what lies ahead.
Phase 1 (Weeks 0-2): Post-Operative Relief marks the period immediately following surgery. Patients experience a mix of excitement about their decision combined with visible healing signs including redness, swelling, and scabbing. The transplanted hair shafts remain visible, creating an initial preview of coverage.
Phase 2 (Weeks 2-8): Shock Loss Anxiety represents the most psychologically challenging period. During this “valley,” appearance may temporarily worsen as transplanted hair shafts shed. Understanding that this is a normal biological response—not a sign of failure—proves essential for mental wellbeing.
Phase 3 (Months 6-18): Patience-Testing Maturation brings visible progress, though waiting for final density and texture normalization requires continued patience. Recognizing these emotional phases helps patients navigate the journey with appropriate expectations.
The Immediate Post-Operative Period: Days 1-10
The initial recovery window spans approximately 5-7 days, during which swelling, redness, and scabbing represent normal healing responses. Scabs typically form over recipient sites within the first 48 hours and naturally fall off by days 7-10 as the body’s protective mechanism completes its function.
During this phase, patients should document several visual markers:
- Recipient site redness patterns
- Scab formation and progression
- Donor area appearance and healing
- Overall swelling distribution
Normal healing includes mild discomfort, temporary numbness, and pink coloration around grafts. Concerning signs requiring medical attention include persistent bleeding beyond 24 hours, severe swelling affecting vision, or signs of infection such as pus, fever, or increasing pain after day three.
Importantly, while transplanted hair shafts remain visible during this period, the follicles beneath the surface are already entering their dormancy phase—a necessary step in the regeneration process.
The Shock Loss Valley: Weeks 2-4
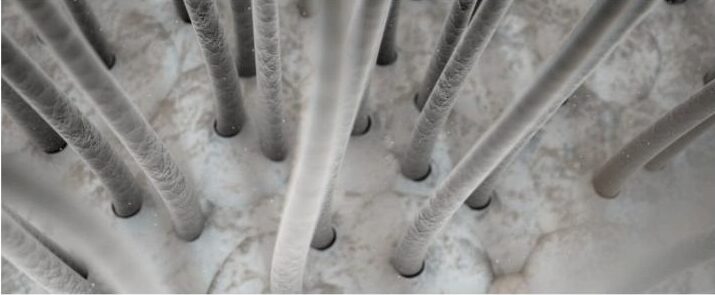
Shock loss affects 30-80% of patients and represents the temporary shedding of transplanted hair shafts while follicles remain intact beneath the scalp surface. This phenomenon occurs because surgical trauma triggers follicles to enter the telogen (resting) phase of the hair growth cycle.
The biological mechanism involves ischemia—temporary reduction of blood supply—combined with the physical stress of extraction and reimplantation. These factors cause follicles to shed their current hair shafts and enter a protective dormant state.
During this phase, patients may appear thinner than before surgery, creating significant psychological distress for those unprepared for this reality. However, hair shaft shedding does not indicate follicle death. The roots remain viable beneath the scalp, preparing for eventual reactivation.
Photography during this phase establishes the “before improvement” baseline, making eventual progress more apparent when comparing images later in the recovery journey.
The Biological WHY: Understanding Follicle Dormancy and Reactivation
The hair growth cycle consists of three distinct phases: anagen (active growth lasting 2-7 years), catagen (transition lasting 2-3 weeks), and telogen (resting lasting approximately 3 months). Understanding this cycle explains why transplanted follicles must enter dormancy before producing new growth.
Surgical trauma triggers a protective telogen phase in transplanted follicles. This response, while frustrating for patients eager to see results, actually demonstrates healthy follicle function. The dormancy period allows follicles to establish blood supply connections in their new location.
Graft survival correlates significantly with ischemia time—the period grafts spend outside the body. Grafts implanted within 2-4 hours demonstrate considerably higher survival rates than those waiting 6+ hours. This underscores the importance of experienced surgical teams who work efficiently to minimize graft exposure time.
Around month three, follicles begin shifting from telogen back to anagen phase, initiating new hair production. Critically, transplanted follicles maintain their genetic DHT resistance—the characteristic that made them suitable donors—ensuring permanent results.
The Waiting Game: Months 2-3 (The ‘Ugly Duckling Phase’)
This period often proves the most difficult psychologically, as patients observe minimal visible progress despite significant time elapsed since surgery. Follicles remain dormant but are actively preparing for anagen reactivation beneath the surface.
Patients should maintain realistic expectations during this phase. Appearance may closely resemble or even appear thinner than pre-surgery baseline. Focusing on healing rather than visible results helps manage frustration.
Even when hair growth isn’t apparent, documenting scalp health improvements—reduced redness, healed donor areas, normalized skin texture—provides evidence of ongoing recovery.
First Signs of Life: Months 3-4
New hair growth typically emerges around month three, though initial hairs appear thin, wispy, and fine. Reduced melanin and keratin production during early growth phases results in lighter coloration and thinner diameter than mature hair will eventually display.
Visual markers during this phase include:
- Fine hair “fuzz” appearing in recipient areas
- Uneven growth patterns as follicles reactivate at different rates
- Possible variation in hair direction or texture
This patchy, irregular appearance is entirely normal. Different follicles reactivate on individual schedules, creating temporary asymmetry that resolves as more follicles enter active growth.
Monthly photography becomes particularly valuable from this point forward, documenting the progressive density improvements that may be difficult to perceive day-to-day.
Building Momentum: Months 4-6
By month six, patients typically achieve approximately 40-50% of final density—the “halfway point” where results become genuinely noticeable. Hair shafts begin thickening as keratin production increases, though texture may still appear wiry or kinky compared to native hair.
Frontal areas generally show more advancement than crown regions during this phase. This differential progress is anatomically normal, not indicative of technique problems.
While patients often feel pleased at this stage, understanding that results are only halfway complete helps maintain appropriate expectations for continued improvement.
The Maturation Plateau: Months 6-12
Understanding the distinction between “popping” and “maturation” proves crucial during this phase. “Popping” refers to new hairs emerging through the scalp surface, while “maturation” describes the thickening, darkening, and texture normalization of existing hairs.
By month nine, patients typically achieve 60-75% of final density with increasingly natural appearance and better blending with native hair. Keratin production continues increasing, gradually thickening hair shafts toward their final diameter.
Progress may appear to slow during this period, though critical maturation processes continue. Hair shaft diameter changes, color saturation deepening, and texture normalization occur gradually over weeks and months.
The Crown Lag Reality: Why Hairline Results Lead Crown Results
An often-overlooked aspect of hair transplant recovery involves the significant difference in maturation timing between frontal and crown areas. Crown results typically lag frontal results by 4-6 months.
Several biological factors contribute to this difference:
- Reduced blood supply in crown regions
- Different growth cycle timing
- Greater surgical trauma due to hair direction complexity
Frontal areas commonly reach maturity around 12 months, while crown regions may require 18+ months for complete maturation. This represents normal anatomy rather than surgical failure.
Patients benefit from maintaining separate documentation tracking for frontal versus crown progress, allowing accurate assessment of each region’s development.
Final Results: Months 9-18
The 12-month milestone typically reveals 85-95% of final results in frontal areas. Hair shafts reach full diameter, color matches native hair, and texture normalizes to blend seamlessly with existing growth.
Crown and mid-scalp areas continue maturing through month 18, eventually achieving comparable results to frontal regions. Overall, 90-95% of transplanted follicles survive and produce hair when procedures are performed by qualified professionals.
Patient satisfaction data demonstrates the procedure’s effectiveness, with studies showing average satisfaction ratings of 8.3 out of 10 at three years post-procedure.
Visual Documentation Best Practices
Consistent photography enables accurate progress assessment. A standardized protocol should include:
Required views: Frontal, top-down, both sides, crown, and close-ups of recipient areas
Consistency factors: Same lighting conditions, identical camera angles, consistent head positioning, uniform background
Timing: Baseline (pre-operative), immediate post-operative, then monthly from month three onward
Using the same location, lighting, and camera settings for every session ensures accurate comparison across the recovery timeline.
Supporting the Timeline: Adjunctive Treatments
Several treatments can support the natural recovery process, though none replace the required patience for biological maturation.
Finasteride demonstrates 85%+ stabilization or improvement after five years, protecting native hair during the recovery period when transplanted areas are still maturing.
Minoxidil may support transplanted follicles and potentially accelerate the growth phase transition.
PRP therapy and low-level laser therapy offer additional support options, while newer technologies like Alma TED provide needle-free delivery of growth serums.
These treatments complement rather than accelerate the natural timeline—understanding this prevents unrealistic expectations.
When to Contact a Surgeon
Distinguishing normal healing from concerning signs helps patients know when professional consultation is warranted.
Normal signs: Temporary redness lasting 2-3 weeks, shock loss during weeks 2-4, uneven growth patterns through month 6, crown lag compared to frontal areas
Concerning signs requiring consultation: Persistent redness beyond 3-4 weeks, widespread shedding extending well beyond the shock loss phase, signs of infection, complete absence of growth by month 5
Follow-up appointments at 6 and 12 months allow professional assessment of progress. Qualified surgeons provide ongoing support throughout the entire recovery timeline.
Realistic Expectations and Individual Variation
Evidence-based success rates demonstrate 90-95% graft survival when procedures are performed by qualified professionals. However, 100% density is rarely achieved—typical coverage represents 90-95% of transplanted follicles producing hair.
Individual variation factors affecting timeline progression include:
- Age and overall health status
- Hair characteristics (color, texture, curl pattern)
- Healing capacity and skin type
- Lifestyle factors including nutrition, stress levels, sleep quality, and smoking status
First-time procedures typically require an average of 2,347 grafts, while subsequent procedures need approximately 1,637 grafts according to current industry data.
The Importance of Surgeon Expertise
Surgical technique directly impacts graft survival and timeline outcomes. Ischemia time, graft handling precision, and placement depth all influence how quickly and successfully follicles establish themselves.
Board-certified surgeons with specialized hair restoration training understand the technical nuances that maximize graft viability. Surgical technicians with extensive experience ensure consistent handling throughout lengthy procedures.
Proper technique minimizes trauma and maximizes follicle survival, directly impacting timeline outcomes and final results.
Conclusion
The hair transplant timeline represents a journey requiring patience through three distinct emotional phases. Understanding the biological processes behind shock loss, dormancy, and maturation helps manage expectations and reduce anxiety during challenging periods.
Key takeaways include: shock loss is temporary and expected, crown lag is anatomically normal, and full maturation requires the complete 12-18 month timeline. Monthly photographic documentation tracks subtle progressive changes that may be imperceptible day-to-day.
With 90-95% graft survival rates and high patient satisfaction, hair transplantation represents an effective solution for hair loss. Focusing on the long-term transformation rather than daily fluctuations helps patients navigate the waiting periods with confidence.
Begin Your Hair Restoration Journey with Confidence
For those considering hair restoration, Hair Transplant Specialists offers comprehensive consultations to discuss personalized timelines and expectations. Their state-of-the-art facilities in Eagan, Minnesota provide a luxury patient experience with board-certified surgeons including Dr. Sharon Keene, former President of the International Society of Hair Restoration Surgery.
With transparent all-inclusive pricing and financing options starting at $150 per month, patients can begin their transformation with a team committed to guiding them through every phase of the journey. Contact Hair Transplant Specialists at (651) 393-5399 or visit INeedMoreHair.com to schedule a consultation and take the first step toward restored confidence.