Hair Transplant Graft Survival Rate: The Ischemia Time & Transection Protocol That Separates Elite Surgeons
When researching hair transplant procedures, patients encounter the same reassuring statistic repeatedly: “90-95% graft survival rate.” This single number appears across clinic websites, marketing materials, and consultation discussions as if it represents a universal standard. However, this figure obscures a critical reality—graft survival is not a single metric but the outcome of three distinct quality benchmarks that vary dramatically between practitioners.
The difference between a procedure that achieves 95%+ survival and one that falls below 85% comes down to three measurable factors: transection rate during extraction, ischemia time management, and storage protocol precision. High-volume clinics and inexperienced surgeons frequently compromise one or more of these metrics, delivering results that fall short of marketed claims despite technically performing the same procedure.
Understanding these three pillars empowers patients to evaluate surgeons beyond surface-level statistics. Elite practitioners achieve transection rates below 2%, maintain ischemia times under four hours, and employ hypothermic storage protocols—benchmarks that require both surgical expertise and sophisticated facility infrastructure.
Understanding Hair Transplant Graft Survival Rate: Beyond the 90-95% Marketing Claim
Graft survival rate refers to the percentage of transplanted follicles that successfully establish blood supply and produce visible hair 12-18 months post-procedure. Modern hair transplant techniques—both FUE (Follicular Unit Extraction) and FUT (Follicular Unit Transplantation)—achieve comparable survival rates of 90-95% when performed by experienced surgeons. DHI (Direct Hair Implantation) reports slightly higher rates of 90-97% due to minimal time grafts spend outside the body.
However, the commonly cited 90-95% range represents ideal conditions in controlled research settings, not necessarily real-world outcomes across all clinics. Studies confirm that survival rates exceeding 90% are achievable in non-smoking, healthy individuals when tracked 12-18 months post-surgery—but this requires optimization of multiple technical factors simultaneously.
Patients must distinguish between three separate outcome measures that clinics often conflate:
- Graft survival: The biological viability of transplanted follicles
- Aesthetic success: Visual density and natural appearance
- Patient satisfaction: Meeting individual expectations
A procedure may achieve high graft survival while still disappointing patients aesthetically if hairline design or density distribution falls short. Conversely, technically excellent results may not satisfy patients with unrealistic expectations. Elite surgeons address all three dimensions, but graft survival forms the biological foundation upon which aesthetic and satisfaction outcomes depend.
The Three Quality Metrics That Determine Graft Survival Rate
The separation between elite surgeons and average practitioners lies not in the procedures they perform but in how precisely they execute three interconnected quality metrics. Excellence in one area cannot compensate for deficiency in another—a surgeon with exceptional extraction precision still compromises outcomes if grafts sit in suboptimal storage for extended periods.
These metrics require both individual surgical skill and facility infrastructure. Dual surgical suites enabling parallel extraction and implantation, experienced technician teams, and standardized protocols all contribute to consistent performance across all three dimensions.
Metric #1: Transection Rate During Extraction (The Precision Benchmark)
Transection rate measures the percentage of follicles damaged or severed during extraction, rendering them non-viable before transplantation even begins. This represents the most objective quality control metric in hair restoration—unlike subjective aesthetic assessments, transection can be measured precisely.
Quality benchmarks for transection rates:
- Acceptable surgeons: Below 5%
- Good surgeons: Below 3%
- Elite surgeons: Consistently below 2%
Damaged follicles cannot be transplanted, reducing the total available grafts and potentially requiring additional procedures to achieve desired density. For patients paying per graft, high transection rates mean paying for follicles that never had a chance to grow.
Technical factors affecting transection include extraction angle precision, punch size selection, and understanding of follicle curvature. This last factor proves especially critical for Afro-textured hair, which has curved follicle structures that increase transection risk and result in slightly lower survival rates of 80-90%.
Surgeon and technician experience serves as the primary determinant of transection rates. Surgical technicians with over 18 years of experience achieve sub-2% transection rates through refined extraction technique developed across thousands of procedures. This level of precision requires pattern recognition and motor skills that only develop over many years of focused practice.
Metric #2: Ischemia Time Management (The Critical Window)
Ischemia time refers to the period grafts spend outside the body without blood supply, from the moment of extraction to implantation. This represents perhaps the most overlooked factor in patient education despite its dramatic impact on outcomes.
Critical ischemia thresholds:
- Grafts implanted within 2-4 hours: Significantly higher survival
- Grafts waiting 6+ hours: Progressive survival decline
- Maximum viable window: 12-14 hours with optimal preservation
During ischemia, grafts experience multiple biological stresses. Dehydration poses the most immediate threat—graft death can occur in as little as 3-16 minutes in dry environments without proper hydration protocols. Grafts also undergo metabolic stress from oxygen deprivation and ischemia-reperfusion injury when blood supply is restored.
Ischemia time increases in predictable circumstances: large procedures requiring 3,000+ grafts, single-surgeon practices where one person handles all extraction and implantation, insufficient support staff, and facilities lacking dual surgical suites. When extraction must complete before implantation begins, early-extracted grafts may wait hours before placement.
Advanced practices address this challenge through infrastructure design. With two state-of-the-art surgical suites, extraction and implantation can occur simultaneously—grafts move from donor area to recipient site with minimal delay even in large procedures. This parallel processing capability represents a significant advantage over single-suite practices where sequential workflow extends total procedure time.
Contrast this with high-volume overseas clinics performing multiple procedures daily. When procedures extend 8-10 hours to accommodate large graft counts, later grafts spend excessive time outside the body, compromising survival regardless of extraction precision or storage quality.
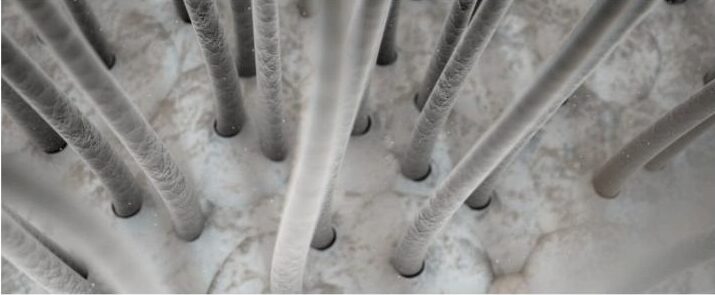
Metric #3: Storage Protocol Precision (The Preservation Science)
Storage protocol encompasses the temperature, hydration, and preservation solution used to maintain graft viability during the procedure. For longer procedures, storage quality becomes increasingly determinative of outcomes.
Three components of optimal storage:
- Temperature control: Hypothermic conditions of 4-8°C slow metabolic rate and preserve cellular integrity
- Hydration maintenance: Preventing the 3-16 minute dehydration window that causes graft death
- Preservation solution chemistry: The medium in which grafts are stored
Preservation solutions exist on a quality hierarchy. Basic saline represents the minimum acceptable standard. Specialized preservation media like HypoThermosol with ATP demonstrate superior results, particularly for procedures exceeding four hours. PRP (Platelet-Rich Plasma) enriched solutions represent the evidence-based enhancement tier—research indicates 15-20% improvement in graft survival and reduced shock loss when PRP is incorporated into storage and implantation protocols.
Protocol precision matters exponentially more in longer procedures. Grafts extracted in the first hour of a six-hour procedure require superior preservation to maintain viability until implantation. Elite practices maintain strict temperature monitoring, regular solution refreshment, and standardized handling protocols that prevent quality drift as procedures progress and team fatigue accumulates.
Why Facility Infrastructure and Team Experience Matter as Much as Surgeon Skill
A common misconception holds that surgeon skill alone determines hair transplant outcomes. While surgeon expertise remains essential, the three quality metrics require infrastructure and team capabilities that extend beyond any individual practitioner.
Infrastructure requirements for metric optimization:
- Dual surgical suites enabling parallel extraction and implantation
- Temperature-controlled graft storage systems
- Experienced technician teams (not just the surgeon)
- Standardized protocols refined through high case volumes
Leading practices exemplify this comprehensive approach with two state-of-the-art surgical suites, surgical technicians with over 18 years of experience, and protocols refined over 100+ combined years of practice among the team.
Single-suite practices face inherent ischemia time challenges even when staffed by skilled surgeons. When extraction must complete before implantation begins, the sequential workflow guarantees extended out-of-body time for early grafts.
The overseas clinic risk extends beyond individual surgeon quality. High-volume facilities performing four to six procedures daily cannot provide the attention to storage protocols and ischemia time management that smaller-volume, quality-focused practices maintain. When technicians manage multiple simultaneous procedures, protocol adherence inevitably suffers.
Extraction precision depends heavily on technician skill, not just surgeon oversight. Over 18 years of experience among skilled technicians translates to refined technique across thousands of procedures—pattern recognition and motor precision that directly impact transection rates.
Patient Factors That Influence Graft Survival Rate
Patient characteristics interact with the three quality metrics to determine final outcomes. Some factors are modifiable; others require surgical adaptation.
Modifiable factors:
- Smoking status: Significantly reduces graft survival through impaired microcirculation
- Diabetes control: Poorly controlled blood sugar compromises healing
- Post-operative care adherence: Grafts become secure 10-14 days post-transplant as revascularization occurs within 3-7 days
Non-modifiable factors:
- Hair texture: Afro-textured hair’s curved follicle structure increases transection risk
- Scalp health: Scarring or poor blood supply affects implantation success
- Genetic healing capacity: Individual variation in tissue repair
Graft density creates an important trade-off. Higher density (50+ grafts per cm²) reduces survival to approximately 84% compared to 95%+ at 30 grafts per cm² due to competition for blood supply during revascularization. Elite surgeons balance density goals with survival optimization, sometimes recommending staged procedures rather than compromising per-graft survival.
In healthy, non-smoking individuals with proper post-operative care, survival rates exceeding 90% are consistently achievable when all three quality metrics are optimized.
How to Evaluate a Surgeon’s Quality Metrics During Consultation
Informed patients can assess the three quality metrics through specific consultation questions. Surgeons confident in their outcomes welcome these inquiries; evasive responses signal potential concerns.
Transection rate questions:
- “What is your average transection rate?” (Target: below 3%, ideally below 2%)
- “How do you measure and track transection rates?”
- “What is your technician team’s experience level?”
Ischemia time questions:
- “How long will my grafts spend outside my body?”
- “Do you have multiple surgical suites to enable parallel processing?”
- “What is your typical procedure duration for my graft count?”
Storage protocol questions:
- “What preservation solution do you use?”
- “How do you maintain graft temperature during the procedure?”
- “Do you offer PRP therapy as part of the transplant protocol?”
Red flags indicating quality concerns:
- Vague answers about survival rates without supporting data
- No discussion of transection rates
- Single-suite facilities for large procedures
- Procedures scheduled back-to-back suggesting rushed timelines
Green flags indicating quality focus:
- Specific transection rate data with tracking methodology
- Detailed explanation of storage protocols
- Experienced technician teams (15+ years)
- Dual surgical suite infrastructure
- Willingness to discuss all three metrics transparently
The Hair Transplant Specialists Approach to Maximizing Graft Survival
Hair Transplant Specialists optimizes all three quality metrics through integrated infrastructure, team expertise, and refined protocols.
Transection rate optimization relies on surgical technicians with over 18 years of experience achieving elite sub-2% rates through extraction precision developed across thousands of procedures.
Ischemia time management leverages two state-of-the-art surgical suites enabling parallel extraction and implantation, minimizing out-of-body time even in large 3,000+ graft procedures.
Storage protocol precision employs hypothermic storage systems, specialized preservation solutions, and standardized handling protocols refined over 100+ combined years of practice.
The team includes board-certified surgeons Dr. Sharon Keene, former President of the International Society of Hair Restoration Surgery, and Dr. Roy Stoller with over 20 years of individual experience. Their proprietary Microprecision Follicular Grafting® technique represents the synthesis of these quality metrics into a systematic approach to maximizing survival.
Critically, procedures are designed around optimal graft survival rather than maximizing daily patient volume—a philosophy that prioritizes outcomes over throughput.
Conclusion
Graft survival rate is not a single number but the outcome of three distinct quality metrics that must all be optimized simultaneously. Elite surgeons achieve transection rates below 2%, maintain ischemia times under four hours, and employ precision storage protocols with hypothermic preservation and evidence-based enhancements like PRP therapy.
These metrics require both surgeon expertise and facility infrastructure. Dual surgical suites, experienced technician teams, and standardized protocols are not optional enhancements—they are prerequisites for consistently achieving the 90-95% survival rates that clinics routinely claim.
The commonly cited survival statistics represent what is achievable under optimal conditions, not what every clinic delivers. Informed patients who ask specific questions about transection rates, ischemia time, and storage protocols during consultations position themselves to select surgeons who deliver superior outcomes.
Hair transplant success is determined in the technical details of extraction precision, time management, and preservation science. Patients who understand these factors can look beyond marketing claims to identify practitioners whose protocols and infrastructure support the results they promise.
Schedule a Consultation
Hair Transplant Specialists invites prospective patients to experience the difference that over 18 years of technician experience, dual surgical suites, and protocols refined over 100+ combined years of practice deliver.
Contact Information:
- Phone: (651) 393-5399
- Location: 2121 Cliff Dr. Suite 210, Eagan, MN 55122
- Website: INeedMoreHair.com
During consultations, patients are encouraged to ask about transection rates, ischemia time management, and storage protocols. The team welcomes the opportunity to discuss the technical details that separate elite outcomes from average results.
Virtual tours of the state-of-the-art dual surgical suites are available online. Flexible financing options start at $150 per month with transparent, all-inclusive pricing and no hidden fees.